Clinical practice guidelines rely heavily on results from randomized controlled trials (RCTs), which is the gold standard for medical research. RCTs produce evidence considered to be of the highest quality. Because RCTs are resource intensive and costly, they are typically of relatively short duration, commonly lasting for around one year.
Currently there are only a few RCTs investigating the effects of testosterone therapy for a duration of 3 years [1-4], and medical societies have long been urging for more long-term trials evaluating the safety and efficacy of testosterone therapy.[5-7]
On August 11th 2015 a notable 3-year long RCT was published in JAMA (Journal of the American Medical Association), which attracted a lot of attention.[8] While interpreted by many as showing that testosterone therapy does not confer any benefits on atherosclerosis, sexual function and quality of life, a closer look at the raw data actually shows two important positive results…
Key Points
– The results of the 3-year long JAMA study were reported in the abstract as mainly neutral, concluding that testosterone therapy did not affect markers of atherosclerosis (intima-media thickness and coronary artery calcium score), nor improve overall sexual function or health-related quality of life.
– As expected, hematocrit and PSA levels increased more in the testosterone group, but values stayed largely within the normal range.
– An important problem of the study, also not mentioned in the abstract, was that testosterone levels declined over time, despite the dose-adjustments aiming to achieve testosterone levels between 500 and 900 ng/dL (suggesting low adherence and sub-optimal testosterone therapy).
– Two important positive outcomes, which were not mentioned in the study abstract, were:
* The number of subjects reporting adverse events or serious adverse events did not differ between testosterone and placebo groups. This confirms that testosterone therapy is safe, even in men over 60 years of age.
* In men not taking statins, one marker of atherosclerosis (coronary artery calcium) was significantly lower in the testosterone group than in the placebo group.
What is known
Evidence for and against testosterone therapy is conflicting. Previous RCTs have shown an increase (in men with pre-existing morbidities) [9] or no increase in adverse events [10], and retrospective studies show either increased [11, 12] or reduced [13, 14] risk of stroke and MI (myocardial infarction). Three other retrospective studies even show increased longevity (reduced mortality risk) with testosterone therapy.[14-16]
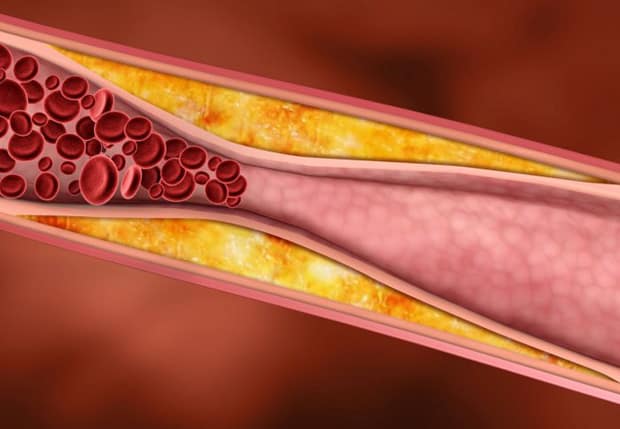
Coronary heart disease is a clinical manifestation of atherosclerosis.[17] Two common techniques for measuring subclinical atherosclerosis – which reflects lifetime risk factor exposure [18] – is carotid intima-media thickness (CIMT) and coronary artery calcium (CAC).
CIMT has been validated as a measure of the atherosclerotic burden [19] and of the risk for cardiovascular events.[20] CAC reflects atherosclerotic plaque burden, because calcium deposits are related to the lipid and apoptotic remnants of the plaque.[21]
Many studies show that low testosterone levels are associated with increased atherosclerotic burden (measured by CIMT) [22-32], and clinical trials of testosterone therapy have shown significant reductions in CIMT.[33, 34]
What this study adds
The new study Basaria et al. aimed to determine the effect of testosterone administration on subclinical atherosclerosis progression in older men with low or low-normal testosterone levels.[8]
156 participants were randomized to receive 7.5 g of 1% testosterone gel and 152 were randomized to receive placebo gel daily for 3 years. The dose was adjusted to achieve testosterone levels between 500 and 900 ng/dL (see commentary below).
Results showed that testosterone therapy did not affect markers of atherosclerosis (intima-media thickness and coronary artery calcium score), nor improve overall sexual function or health-related quality of life. Testosterone therapy elevated hematocrit and PSA levels increased more in the testosterone group, but values stayed largely within the normal range.
Two important positive outcomes, which were not mentioned in the study abstract (or media headlines), were:
* The number of subjects reporting adverse events or serious adverse events did not differ between testosterone and placebo groups. This confirms that safety is not a major issue with testosterone therapy.
* In men not taking statins, one marker of atherosclerosis (coronary artery calcium) was significantly lower in the testosterone group than in the placebo group.
Commentary
The finding that hematocrit and PSA elevations largely stayed within normal range, and that the number of participants reporting adverse events or serious adverse events did not differ between groups, is great news. Especially considering that this is one of the few long-term studies in men of advanced age (mean age 67 years). Even though testosterone levels dropped as the study progressed, if testosterone therapy really was as dangerous as screaming media headlines want us to believe, this study would not have reported that serious adverse events did not differ between testosterone treated and placebo groups (testosterone levels were above 600 ng/dL for the first 18 months).
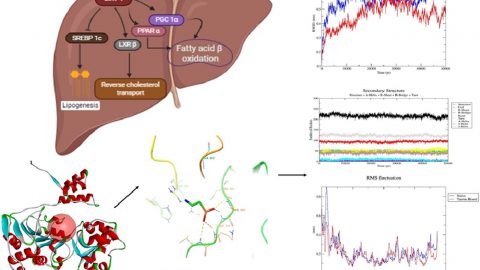
There are several issues with this study. An important methodological problem – also not mentioned in the abstract – was that testosterone levels declined over time despite dose-adjustments aiming to achieve testosterone levels between 500 and 900 ng/dL. This indicates low adherence and sub-optimal testosterone therapy. Data for achieved testosterone were only reported graphically, as opposed to numerically, making it harder (on purpose?) to see actual absolute changes in testosterone levels:
Figure from Basaria, S., et al., Effects of Testosterone Administration for 3 Years on Subclinical Atherosclerosis Progression in Older Men With Low or Low-Normal Testosterone Levels: A Randomized Clinical Trial. JAMA, 2015. 314(6): p. 570-81.
Nevertheless, looking at the graphs (published as Figure 2 in the original paper), the following approximate testosterone levels were achieved:
6 months: total testosterone: 640 ng/dL free testosterone: 120 pg/mL
18 months: total testosterone: 600 ng/dL free testosterone: 110 pg/mL
36 months: total testosterone: 460 ng/dL free testosterone: 85 pg/mL
This clearly shows that the study failed to achieve testosterone levels between 500 and 900 ng/dL for the total duration of the study, especially after the 18 month mark, after which levels in both total and free testosterone drastically plummeted. This was not reported in the study abstract. Thus, it is still possible that effective testosterone therapy (that maintains therapeutic testosterone levels throughout the treatment duration) may reduce atherosclerosis progression.
Another important issue is that two thirds of the subjects in the testosterone group were taking statins. It is well-documented that statins [35-37] – which are widely prescribed for dyslipidemia – significantly reduce testosterone levels. Hence, it is possible that statins may counteract the achievement of therapeutic testosterone levels and the beneficial effects with testosterone therapy, which in this case would be the rate of progression (or regression) of subclinical atherosclerosis.
The placebo group experienced a marked reduction in cholesterol levels (both total and LDL cholesterol). As medication dosages were not reported, this raises the question if the placebo group increased their statin dose. If so, this would explain both the cholesterol reductions and the possible lack of effect on subclinical atherosclerosis.
Regarding safety, it should be pointed out that the hematocrit and PSA elevations in the testosterone group stayed within the normal range, and are to be expected with testosterone therapy. More importantly, the number of subjects reporting adverse events or serious adverse events did not differ between testosterone and placebo groups. These are solid data supporting the concept that testosterone therapy does not increase atherosclerosis / cardiovascular risk – and may actually reduce it in men who are not taking statins – and confirms that long-term testosterone therapy is safe.
Regarding sexual function, it has to be underscored that the study subjects were selected solely based on testosterone levels, without requirement for symptoms. Thus, as baseline sexual function already was good – as indicated by the greater baseline scores for sexual desire and orgasmic function – it is unrealistic to expect sexual function or quality of life to improve. Nonetheless the curves for sexual symptoms are all better numerically in the testosterone group than in the placebo group, although differences were not significant. This is probably because the subgroup with sexual symptoms (e.g., diminished libido) did improve, whereas those with normal libido could not be made “more normal”. It is also interesting to note that the sexual function parameters tended to decline in parallel with the declines in testosterone levels.
Finally, it is critical to remember that each androgen dependent effect has its own testosterone threshold.[38] Lack of improvement in sexual function and quality of life – two outcomes that require only relatively low testosterone levels [39] – does not mean that other effects (such as subclinical atherosclerosis, body fat loss and muscle gain) would not improve from testosterone therapy that achieves a higher and sustained therapeutic elevation in testosterone levels. In fact, previous studies that did achieve therapeutic testosterone levels for a sufficient duration have shown reductions in subclinical atherosclerosis [33, 34], and previous 3 year-year long testosterone therapy studies did report significant body fat loss and increases in lean body mass (muscle) gain.[2, 40]
———————————————————————————————————————————————–
About Monica Mollica > www.Ageless.Fitness

Monica Mollica holds a Master degree in Nutrition from the University of Stockholm / Karolinska Institue, Sweden. She has also done PhD level course work at renowned Baylor University, TX.
Having lost her father in a lifestyle-induced heart attack at an age of 48, she is a strong advocate of primary prevention and early intervention, and the development of lifestyle habits for health promotion at all ages.
Today, Monica is sharing her solid medical research insights, real life hands on experience, and passion for health and fitness by offering nutrition / supplementation / exercise / health consultation services, and working as a medical writer specializing in health promotion, fitness and anti-aging.
She is currently in the process of writing a book on testosterone, covering health related issues for both men and women.
———————————————————————————————————————————————–
References:
1. Amory, J.K., et al., Exogenous testosterone or testosterone with finasteride increases bone mineral density in older men with low serum testosterone. J Clin Endocrinol Metab, 2004. 89(2): p. 503-10.
2. Page, S.T., et al., Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J Clin Endocrinol Metab, 2005. 90(3): p. 1502-10.
3. Snyder, P.J., et al., Effect of testosterone treatment on bone mineral density in men over 65 years of age. J Clin Endocrinol Metab, 1999. 84(6): p. 1966-72.
4. Snyder, P.J., et al., Effect of testosterone treatment on body composition and muscle strength in men over 65 years of age. J Clin Endocrinol Metab, 1999. 84(8): p. 2647-53.
5. Bhasin, S., et al., Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2010. 95(6): p. 2536-59.
6. Dohle, G.R., et al., EAU Guidelines on Male Hypogonadism. 2012, European Association of Urology
7. Wang, C., et al., Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl, 2009. 30(1): p. 1-9.
8. Basaria, S., et al., Effects of Testosterone Administration for 3 Years on Subclinical Atherosclerosis Progression in Older Men With Low or Low-Normal Testosterone Levels: A Randomized Clinical Trial. JAMA, 2015. 314(6): p. 570-81.
9. Basaria, S., et al., Adverse events associated with testosterone administration. N Engl J Med, 2010. 363(2): p. 109-22.
10. Srinivas-Shankar, U., et al., Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab, 2010. 95(2): p. 639-50.
11. Vigen, R., et al., Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA, 2013. 310(17): p. 1829-36.
12. Finkle, W.D., et al., Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One, 2014. 9(1): p. e85805.
13. Baillargeon, J., et al., Risk of Myocardial Infarction in Older Men Receiving Testosterone Therapy. Ann Pharmacother, 2014. 48(9): p. 1138-1144.
14. Sharma, R., et al., Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men. Eur Heart J, 2015.
15. Shores, M.M., et al., Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab, 2012. 97(6): p. 2050-8.
16. Muraleedharan, V., et al., Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrinol, 2013. 169(6): p. 725-33.
17. Toth, P.P., Subclinical atherosclerosis: what it is, what it means and what we can do about it. Int J Clin Pract, 2008. 62(8): p. 1246-54.
18. Erbel, R. and M. Budoff, Improvement of cardiovascular risk prediction using coronary imaging: subclinical atherosclerosis: the memory of lifetime risk factor exposure. Eur Heart J, 2012. 33(10): p. 1201-13.
19. Taylor, A.J., et al., ARBITER: Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol: a randomized trial comparing the effects of atorvastatin and pravastatin on carotid intima medial thickness. Circulation, 2002. 106(16): p. 2055-60.
20. Lorenz, M.W., et al., Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation, 2007. 115(4): p. 459-67.
21. Schmermund, A., S. Mohlenkamp, and R. Erbel, Coronary artery calcium and its relationship to coronary artery disease. Cardiol Clin, 2003. 21(4): p. 521-34.
22. De Pergola, G., et al., Free testosterone plasma levels are negatively associated with the intima-media thickness of the common carotid artery in overweight and obese glucose-tolerant young adult men. Int J Obes Relat Metab Disord, 2003. 27(7): p. 803-7.
23. Dorr, M., H. Wallaschofski, and N. Friedrich, Association of low total testosterone levels and prevalent carotid plaques: result of the study of health in Pomerania. Eur J Epidemiol, 2009. 24(7): p. 389-91.
24. Fu, L., Q.P. Gao, and J.X. Shen, Relationship between testosterone and indexes indicating endothelial function in male coronary heart disease patients. Asian J Androl, 2008. 10(2): p. 214-8.
25. Fukui, M., et al., Association between serum testosterone concentration and carotid atherosclerosis in men with type 2 diabetes. Diabetes Care, 2003. 26(6): p. 1869-73.
26. Makinen, J., et al., Increased carotid atherosclerosis in andropausal middle-aged men. J Am Coll Cardiol, 2005. 45(10): p. 1603-8.
27. Muller, M., et al., Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation, 2004. 109(17): p. 2074-9.
28. Soisson, V., et al., Low plasma testosterone and elevated carotid intima-media thickness: importance of low-grade inflammation in elderly men. Atherosclerosis, 2012. 223(1): p. 244-9.
29. Svartberg, J., et al., Low testosterone levels are associated with carotid atherosclerosis in men. J Intern Med, 2006. 259(6): p. 576-82.
30. Tsujimura, A., et al., Low serum free testosterone level is associated with carotid intima-media thickness in middle-aged Japanese men. Endocr J, 2012. 59(9): p. 809-15.
31. van den Beld, A.W., et al., Endogenous hormones and carotid atherosclerosis in elderly men. Am J Epidemiol, 2003. 157(1): p. 25-31.
32. Vikan, T., et al., Endogenous testosterone and the prospective association with carotid atherosclerosis in men: the Tromso study. Eur J Epidemiol, 2009. 24(6): p. 289-95.
33. Francomano, D., et al., Effects of testosterone undecanoate replacement and withdrawal on cardio-metabolic, hormonal and body composition outcomes in severely obese hypogonadal men: a pilot study. J Endocrinol Invest, 2014. 37(4): p. 401-11.
34. Aversa, A., et al., Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebo-controlled study. J Sex Med, 2010. 7(10): p. 3495-503.
35. Schooling, C.M., et al., The effect of statins on testosterone in men and women, a systematic review and meta-analysis of randomized controlled trials. BMC Med, 2013. 11: p. 57.
36. Corona, G., et al., The effect of statin therapy on testosterone levels in subjects consulting for erectile dysfunction. J Sex Med, 2010. 7(4 Pt 1): p. 1547-56.
37. Cohen, P.G., Statins and male hypogonadism. J Sex Med, 2011. 8(6): p. 1826.
38. Sattler, F., et al., Testosterone threshold levels and lean tissue mass targets needed to enhance skeletal muscle strength and function: the HORMA trial. J Gerontol A Biol Sci Med Sci, 2011. 66(1): p. 122-9.
39. Zitzmann, M., S. Faber, and E. Nieschlag, Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Metab, 2006. 91(11): p. 4335-43.
40. Wang, C., et al., Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab, 2000. 85(8): p. 2839-53.







I been on therapy for 3 years, first was the cream, I was 250 up to 550, Then the shot, which put at
1200. I was super man. When I stopped the shot I went back down. Now I take one shot every 3 weeks, I will let you know, Thanks joe
Every man on TRT needs to find his own unique optimal T levels. A good guideline is to elevate T levels to the point (right before) where HDL starts to drop.