Some of the most popular supplements today are the so called pre-workout nitric oxide (NO) boosters [1, 2]. These contain a panoply of ingredients, but one the main ones is arginine. The rationale goes that L-arginine is a precursor to nitric oxide (NO) and NO is a potent vasodilator [3, 4] Theoretically this would increase blood flow and nutrient/oxygen delivery to exercising muscles and thereby boost performance, as well as recovery.
While it is true that L-arginine supplementation mat be beneficial for various clinical populations (see below), studies in healthy adults have not unequivocally supported the marketing hype surrounding arginine supplementation and nitric oxide boosters [1, 5, 6]. Here’s why…
Some reasons explaining the inefficacy of arginine supplementation and arginine based “nitric oxide boosters”
Many pre-workout NO boosting supplements rely on the arginine-NO pathway – and a lot of theoretical assumptions. Some reason for the conflicting findings on arginine supplementation are that studies have used different routes of administration (oral vs. intravenous), various forms of L-arginine, varying exercise testing protocols, different subjects (trained vs. untrained, young vs. elderly), and supplement cocktails containing other substances (eg. creatine, beta-alanine, caffeine, carbs etc) which do have performance enhancing effects on their own.
The rationale for L-arginine supplementation is based largely on research using intravenous L-arginine, often at a high dose of 30 g. This has no practical relevance since most, if not all, supplements are taken orally, and in lower doses. In a direct head-to-head comparison of oral and intravenous L-arginine administration, no effect on vasodilatation (widening of blood vessels) or blood flow was found after oral L-arginine supplementation [7]. One reason for this could be the extensive elimination of orally ingested L-arginine due to intestinal arginase activity and its low bioavailability [8]. To circumvent the low bioavailability one would have to ingest a very large dose of L-arginine, which not only has an unpleasant taste, but also can cause gastric problems [9].
The Arginine Paradox
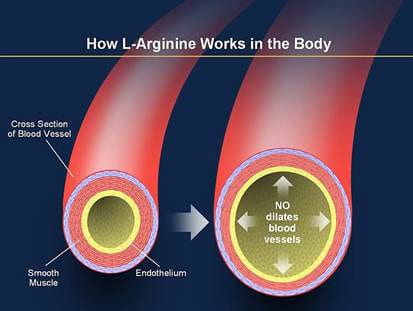
The arginine-NO pathway is controlled by an enzyme called eNOS (endothelial nitric oxide synthase) [10], which converts arginine into NO.[11] The important thing to know is that even in people not taking any arginine supplements, blood level of arginine are already high enough to saturate eNOS. And when an enzyme is saturated with substrate (in this case L-arginine) more substrate won’t have an effect on a reaction. Therefore, if you’re healthy, when you supplement L-arginine (even in large doses) you won’t get more NO from the arginine-NO pathway, simply because L-arginine is not rate-limiting for eNOS.
However, the story is different in clinical conditions like e.g. high blood pressure [12, 13], elevated or abnormal cholesterol levels [14, 15], heart disease [16], insulin resistance [17], diabetes [18, 19] and in the elderly [13, 20, 21]. In those circumstances arginine supplementation may exert beneficial effects, possibly, at least in part, due to increased NO production [13]. Thus, it appears that L-arginine may become a limiting factor for NO synthesis in clinical conditions, but not for healthy individuals.
The term “L-arginine paradox” refers to these specific situations in which L-arginine supplementation indeed does stimulate eNOS activity and NO production, even when blood arginine levels are within the normal range.[5]
One explanation for the L-arginine paradox is the presence of high levels of ADMA (asymmetric dimethylarginine), which is an inhibitor of eNOS [10, 22-24]. ADMA is produced as part of the body’s normal metabolism [25-27], but in clinical conditions ADMA levels are elevated several-fold [24]. In the presence of elevated blood levels of ADMA, eNOS activity is impaired, with a consequent reduced NO production.
How L-arginine supplementation works in the context of elevated ADMA levels
Because ADMA displaces L-arginine and thereby reduces L-arginine availability for eNOS, the ratio of L-arginine to ADMA determines how much of the L-arginine floating around in the blood that will be available for eNOS to use for NO production [28, 29]. In conditions with elevated ADMA levels, L-arginine supplementation will antagonize ADMA by increasing the L-arginine/ADMA ratio, and thereby elevate the availability of L-arginine for eNOS, thus increase NO production [30]. This is supported by studies showing that L-arginine supplementation reverses endothelial (blood vessel) dysfunction caused by high ADMA levels in clinical populations [20, 31-33], and that there exists a direct correlation between the change in L-arginine/ADMA ratio and the change in blood flow mediated dilation (vasodilatation) [8].
How to combat elevated ADMA levels
The importance of ADMA is underscored by the fact that it is considered a novel cardiovascular risk factor [22, 33, 34]. ADMA seems to mediate the negative effects of many risk factors on the eNOS pathway. Therefore, blood ADMA levels have been suggested to be an “Über marker”, or an overall risk factor that reflects the summative effect of multiple risk factors on endothelial and cardiovascular health [26].
Because of this, drug companies are fervently trying to develop drugs that lower ADMA levels. As of this writing there is no ADMA specific drug available. The strongest candidate as an ADMA specific drug is DDAH, the enzyme that naturally breaks down ADMA [27, 35, 36], and whose activity is also impaired in the above mentioned clinical conditions.
DDAH boosting drugs are still in the pre-clinical research phase, and it will likely take many years before they, or any other ADMA lowering drugs, enter the market. However, several well known drugs used for diabetes (metformin, rosiglitazone) and high blood pressure (ACE inhibitors, angiotensin receptor antagonists) have been shown to lower ADMA levels [37-40]. Today, the only non-prescription dietary option is L-arginine supplementation for those in need.
Will L-arginine supplementation benefit you?
If you are insulin resistant (have elevated levels of insulin and/or blood glucose), have high blood pressure, elevated blood cholesterol (or more precisely dyslipidemia, i.e. lipid abnormalities), high homocysteine levels [32], diabetes or cardiovascular disease, and/or have passed middle-age, L-arginine supplementation may work for you in restoring subpar NO production.
In contrast, if you are below middle-age and don’t have any risk factors and, save your money. For you, nitrate or nitrite supplementation, which produces NO via the nitrate–nitrite–NO pathway, is a more promising option. Accumulating research suggests that boosting NO production via the nitrate–nitrite–NO pathway may provide significant health and performance enhancing effects for both those affected by risk factors, as well as healthy people and athlete. For more info on this, see my previous article “Nitrate supplementation – ramp up the less well-known NO synthesizing pathway to boost performance and health“.
References:
1. Bloomer RJ. Nitric oxide supplements for sports. Strength and Conditioning Journal. 2010;32(2):14-20.
2. Bloomer RJ, Farney TM, Trepanowski JF, et al. Comparison of pre-workout nitric oxide stimulating dietary supplements on skeletal muscle oxygen saturation, blood nitrate/nitrite, lipid peroxidation, and upper body exercise performance in resistance trained men. Journal of the International Society of Sports Nutrition. 2010;7:16.
3. Bode-Boger SM, Boger RH, Creutzig A, et al. L-arginine infusion decreases peripheral arterial resistance and inhibits platelet aggregation in healthy subjects. Clin Sci (Lond). 1994;87(3):303-310.
4. Giugliano D, Marfella R, Verrazzo G, et al. The vascular effects of L-Arginine in humans. The role of endogenous insulin. The Journal of clinical investigation. 1997;99(3):433-438.
5. Alvares TS, Meirelles CM, Bhambhani YN, et al. L-Arginine as a potential ergogenic aid in healthy subjects. Sports Med. 2011;41(3):233-248.
6. Wax B, Kavazis AN, Webb HE, et al. Acute L-arginine alpha ketoglutarate supplementation fails to improve muscular performance in resistance trained and untrained men. Journal of the International Society of Sports Nutrition. 2012;9(1):17.
7. Bode-Boger SM, Boger RH, Galland A, et al. L-arginine-induced vasodilation in healthy humans: pharmacokinetic-pharmacodynamic relationship. British journal of clinical pharmacology. 1998;46(5):489-497.
8. Schwedhelm E, Maas R, Freese R, et al. Pharmacokinetic and pharmacodynamic properties of oral L-citrulline and L-arginine: impact on nitric oxide metabolism. British journal of clinical pharmacology. 2008;65(1):51-59.
9. Robinson TM, Sewell DA, Greenhaff PL. L-arginine ingestion after rest and exercise: effects on glucose disposal. Medicine and science in sports and exercise. 2003;35(8):1309-1315.
10. Vallance P, Chan N. Endothelial function and nitric oxide: clinical relevance. Heart. 2001;85(3):342-350.
11. Boger RH, Bode-Boger SM. The clinical pharmacology of L-arginine. Annual review of pharmacology and toxicology. 2001;41:79-99.
12. Pollock JS, Forstermann U, Mitchell JA, et al. Purification and characterization of particulate endothelium-derived relaxing factor synthase from cultured and native bovine aortic endothelial cells. Proceedings of the National Academy of Sciences of the United States of America. 1991;88(23):10480-10484.
13. Gokce N. L-arginine and hypertension. The Journal of nutrition. 2004;134(10 Suppl):2807S-2811S; discussion 2818S-2819S.
14. Higashi Y, Oshima T, Ozono R, et al. Aging and severity of hypertension attenuate endothelium-dependent renal vascular relaxation in humans. Hypertension. 1997;30(2 Pt 1):252-258.
15. Clarkson P, Adams MR, Powe AJ, et al. Oral L-arginine improves endothelium-dependent dilation in hypercholesterolemic young adults. The Journal of clinical investigation. 1996;97(8):1989-1994.
16. Kawano H, Motoyama T, Hirai N, et al. Endothelial dysfunction in hypercholesterolemia is improved by L-arginine administration: possible role of oxidative stress. Atherosclerosis. 2002;161(2):375-380.
17. Adams MR, McCredie R, Jessup W, et al. Oral L-arginine improves endothelium-dependent dilatation and reduces monocyte adhesion to endothelial cells in young men with coronary artery disease. Atherosclerosis. 1997;129(2):261-269.
18. Sydow K, Mondon CE, Cooke JP. Insulin resistance: potential role of the endogenous nitric oxide synthase inhibitor ADMA. Vasc Med. 2005;10 Suppl 1:S35-43.
19. Piatti PM, Monti LD, Valsecchi G, et al. Long-term oral L-arginine administration improves peripheral and hepatic insulin sensitivity in type 2 diabetic patients. Diabetes care. 2001;24(5):875-880.
20. Pieper GM, Siebeneich W, Dondlinger LA. Short-term oral administration of L-arginine reverses defective endothelium-dependent relaxation and cGMP generation in diabetes. European journal of pharmacology. 1996;317(2-3):317-320.
21. Bode-Boger SM, Muke J, Surdacki A, et al. Oral L-arginine improves endothelial function in healthy individuals older than 70 years. Vasc Med. 2003;8(2):77-81.
22. Boger RH, Cooke JP, Vallance P. ADMA: an emerging cardiovascular risk factor. Vasc Med. 2005;10 Suppl 1:S1-2.
23. Cooke JP. ADMA: its role in vascular disease. Vasc Med. 2005;10 Suppl 1:S11-17.
24. Boger RH. Asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, explains the “L-arginine paradox” and acts as a novel cardiovascular risk factor. The Journal of nutrition. 2004;134(10 Suppl):2842S-2847S; discussion 2853S.
25. Sibal L, Agarwal SC, Home PD, et al. The Role of Asymmetric Dimethylarginine (ADMA) in Endothelial Dysfunction and Cardiovascular Disease. Current cardiology reviews. 2010;6(2):82-90.
26. Cooke JP. Asymmetrical dimethylarginine: the Uber marker? Circulation. 2004;109(15):1813-1818.
27. Tran CT, Leiper JM, Vallance P. The DDAH/ADMA/NOS pathway. Atherosclerosis Supplements. 2003;4(4):33-40.
28. Tsikas D, Sandmann J, Savva A, et al. Assessment of nitric oxide synthase activity in vitro and in vivo by gas chromatography-mass spectrometry. Journal of chromatography B, Biomedical sciences and applications. 2000;742(1):143-153.
29. Boger RH, Vallance P, Cooke JP. Asymmetric dimethylarginine (ADMA): a key regulator of nitric oxide synthase. Atherosclerosis Supplements. 2003;4(4):1-3.
30. Bode-Boger SM, Scalera F, Ignarro LJ. The L-arginine paradox: Importance of the L-arginine/asymmetrical dimethylarginine ratio. Pharmacology & therapeutics. 2007;114(3):295-306.
31. Boger RH, Bode-Boger SM, Thiele W, et al. Restoring vascular nitric oxide formation by L-arginine improves the symptoms of intermittent claudication in patients with peripheral arterial occlusive disease. Journal of the American College of Cardiology. 1998;32(5):1336-1344.
32. Sydow K, Schwedhelm E, Arakawa N, et al. ADMA and oxidative stress are responsible for endothelial dysfunction in hyperhomocyst(e)inemia: effects of L-arginine and B vitamins. Cardiovascular research. 2003;57(1):244-252.
33. Boger RH, Bode-Boger SM, Szuba A, et al. Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation. 1998;98(18):1842-1847.
34. Boger RH, Zoccali C. ADMA: a novel risk factor that explains excess cardiovascular event rate in patients with end-stage renal disease. Atherosclerosis Supplements. 2003;4(4):23-28.
35. Cooke JP, Ghebremariam YT. DDAH says NO to ADMA. Arteriosclerosis, thrombosis, and vascular biology. 2011;31(7):1462-1464.
36. Cooke JP. DDAH: a target for vascular therapy? Vasc Med. 2010;15(3):235-238.
37. Asagami T, Abbasi F, Stuelinger M, et al. Metformin treatment lowers asymmetric dimethylarginine concentrations in patients with type 2 diabetes. Metabolism: clinical and experimental. 2002;51(7):843-846.
38. Stuhlinger MC, Abbasi F, Chu JW, et al. Relationship between insulin resistance and an endogenous nitric oxide synthase inhibitor. JAMA : the journal of the American Medical Association. 2002;287(11):1420-1426.
39. Ito A, Egashira K, Narishige T, et al. Renin-angiotensin system is involved in the mechanism of increased serum asymmetric dimethylarginine in essential hypertension. Japanese circulation journal. 2001;65(9):775-778.
40. Delles C, Schneider MP, John S, et al. Angiotensin converting enzyme inhibition and angiotensin II AT1-receptor blockade reduce the levels of asymmetrical N(G), N(G)-dimethylarginine in human essential hypertension. American journal of hypertension. 2002;15(7 Pt 1):590-593.




Seems to me your friend has come up short somewhat, i now have to wait for the next episode i guess to find out about a better nos or vasodiaolator. I imagine she means well and is well intended but, i would and i believe the better majority of us would appreciate a more simpler explanations and not so much high falutent chemical and scientific mumbo jumbo. Much respect Strength and Honor
Hey.
interesting article.
I actually love the fact that you know how to and successfully utilize referencing, along with “nerd speak” for the michaels menten Km, or Vmax equations. I think thats what differentiates someone with the education and knowledge to interpret or analyse results, from your local meat head at the gym who tries to rattle off some big words talking about something he has little to no understanding of.
next weeks pathway should be good.
look forward to it
She’s a scientist, and covers topics using the science. Real science, not Bro science or pseudo science used by some supplement companies and wanna be guru types to market products, so be happy she’s using what you call “scientific mumbo jumbo” to cover the topic. Not everything can be reduced to simple terms and simple reading, some times reading the “high falutent chemical” discussion is a learning opportunity and she does a good job of summarizing the essential take home message for the non scientist.
Great article, Monica can you please make a post about IF.
Thanx
Norm
The Netherlands
I’m 63. I’ve made steady progress through almost a year of training., with no supplements. Would arginine help?
The studies that have shown beneficial effects of arginine supplementation in elderly used people 70 yrs and up. If you don’t have risk factors, then it would be a good supp for you to take. If you don’t have any risk factors, it may or may not help you. You can always try and see how you respond.
Great, and informative article on L-Arginine. Thanks
Jerry
Sorry, -which- situation makes it possibly a good supplement? Both sentences here are if I -do- have risk factors.
Great , informative article on L-Arginine.
what about supplementing with AAKG?
AAKG is facing the same issues as other L-arginine supps. The point is, unless your have a medical condition that negatively impacts eNOS and its NO production, extra arginine won’t do you any good.
Hi Monica, very interesting article and I am amazed by your knowledge & ability to do such detailed research. I have found most of your other articles to be an easy read but must admit to finding this one hard to follow at times. Just a little too much jargon this time. I like the depth of infomration but also appreciate the research being translated into lay-terms that the unresearched person (regular guy like me) can easily interpret and act on. I am really looking forward to part 2 as I have been supplementing with NO precursors and stimulators for a while with varying degrees of success. As you say, these often come with other additives / stimulants so it is hard to tell where the effect is coming from. I am in the UK and at the equivalent of $60-$80 per pack, some of the supplements I’ve been using for a while are by no means cheap. Whether or not I fall into the group for whom NO supplements are beneficial I have no clue. I am 54, with no diabetes, low LDL, OK HDL and resting heart rate of 50bpm. At max cardio, I can sustain a heart rate of 175-180bpm for 8-10 minutes without gassing out so I guess I am reasonably fit. All the best. Gary
Get your homocysteine, blood glucose and insulin levels checked. If they (or any of them) are elevated, you might benefits form L-arginine supplementation.
And what’s your blood pressure?
120/80
You’re in good condition then. My follow-up article will be more relevant for you.
Thanks for the quick reply Monica. I’ve had my homocysteine, blood glucose and insulin levels checked in the last 6-months and all were at acceptable levels. My BP is 120/80. I eat clean & lean, supplement daily with whey protein isolate, ethyl ester creatine, methionine, lysine, A, B, C & E vitamins and liquid fish oils. I don’t drink alcohol and I train 6 times a week, 3 x 1 hour weights sessions (one of which is with a personal trainer) and 3 x 1 hour intense cardio – on alternate days. I’ve also tried a variety of testosterone boosting supplements as at my age it will inevitably be lower but never had any noticeable effect so have stopped wasting my money on those. Love your articles & keep up the great work. Gary
You’re welcome Gary.
Hi Monica, I just wanted to say thank you for your detailed and NO-nonsense article (sorry for the pun) and and the way you publish your sources of information really lends credibility to what you write. Please keep them coming. Great photo too!
Thanks for the compliments 🙂
Once again, awesome article Monica,
I have used it in the past and had stomach problems with it, so i stopped.. and, apart from a better pump, i dint see any other positive aspects to it, i even think that the vasodilatation releases a lot of heat with makes me feel uncomfortable when doing any form of cardio on my workout, either on my warmup or when i reduce rest periods..
I do get a good pump without using anything..
My question is, do you think vasodilatation has any major benefit in terms of muscle building or even performance, or is it just a placebo effect of looking a bit more pumped in the gym mirror ?
Actually, what many people experience after taking NO boosting supplements is paresthesia (a tingling, itching, pins & needles sensation in the skin). This is caused by beta-alanine, which is often added to these products. The beta-alanine induced paresthesia is a side-effect that arises becuase beta-alanine activates nerves in the skin. Is not dangerous, but can be uncomfortable like you said. Some folks mistakenly think this is a sign of the purported NO induced vasodilation. This is unfortunately one reason beta-alanine is frequently added by manufacturers to NO boositng supps.
Whether extra vasodilatation (over and above what is caused by the exercise-induced physiological response) has any major benefit in terms of muscle building and/or performance is still a matter of debate. There are no studies proving this to be the case.
Yes, i know the tingling effect is because of the beta alanine in it, but that didnt feel unconfortable to me, what felt unconfortable was the heat my body produced, i was burning after 5 minutes running, i know most bodybuilders dont include much cardio in their sessions and keep their rest periods high, but i like to do the opposite and finish my workout with a bit of HIIT, so, it was almost impossible, i kept sweating too much.. altough i felt my lactate treshold became better and had a bit more endurance, i dont think it compares to creatine for example..
As you say, unless someone cant get a normal pump from his workout, wich can be a matter of many different factors and should be resolved by addressing those factors directly, i dont see any use for this..
Thanks again for the awesome article and response..
Keep it up !!
Is this heat a side effect from the beta alanine also ? thx
Yes.
Thanks, Monica. It’s good to get the facts and not just marketing type, but disappointing to think we may have been wasting our money while thinking we were doing the right thing.
But what about Agmatine sulfate, which is marketed as being far more effective and available? It is supposedly what arginine is broken down to in the body. Is there any factual information to support these claims? It is far more expensive than arginine or AAKG.
“disappointing to think we may have been wasting our money while thinking we were doing the right thing.”
Michael, had you owned my Body Building Revealed Program, or my newer book The Supplement Bible, you’d know what’s worth using, and what’s not worth using, and save years of wasted time and $$$. Just sayin’… 🙂
While there are some really good supplements backed by scientific research in humans, unfortunately the supplement market is drenched by hyped up hocus-pocus concoctions that lack scientific data to back them up.
Regarding agmatine, white it is true that it is a metabolite of L-arginine, there is are no humans studies whatsoever. Thus it’s potential performance or health effects in humans are mere speculations. The scientific publications available today on agmatine are all based on finding from in vitro (test tube) and rodent studies. Don’t get fooled to waste your money!
I find this an very intersted publication. Greetings Eric Belgium
I’m glad to hear that. 🙂
Hey guys I can tell you first hand that bsn nitrix tabs work but not the way I suspected. I bought this supplement for the muscle pumps and what I got was LOL very suprising. This is the truth guys I never in my life had erections the way I did when on nitrix. To be honset when I had an erection it was so much thicker than usual and harder. I could get off multiple times without going soft. The effects were so crazy my girlfriend totally noticed and said she thought it was alot thicker than normal. Now don’t tell me this product doesn’t work because I know it does at least to that effect. So if anyone has any ED then you should try this product cause I bet it would help you. Please will brink tell me why this?
The take home from the article is that L-arginine supplementation works for certain people who have cardiovascular risk factors (as described in the article).
Problems getting or keeping an erection can be a sign of a health condition that needs treatment, such as heart disease or pre-diabetes/diabetes. Treating the underlying problem may be enough to reverse erectile dysfunction. If you haven’t already, I’d recommend you go in for a comprehensive health check-up.
I really appreciated the in-depth and truly scientific analysis of arginine supplementation. I have an interesting story regarding this supplement. As touted as it may be, we all know it is a completely false and ridiculous claim, i.e., “Muscle Tech”, “MRI” , vasodilator. Science proves otherwise… or does it ?
I am 49, carpenter/painter, have a very demanding and gruelling livelyhood, and have supplemented with arginine for almost ten years. The type that MRI sells , or a good generic equivallent, and there are a few out there…I have found that 4-8 grams daily in the morning and afternoon help ease the constant pain and soreness I experience everyday from my job. It does not make my muscles bigger, but is a great aid in rejuvinating my energy and as an anti-inflammatory agent. I have tried to express this in other forums but have been brushed off. I do not know the scientific reason that arginine benefits me, but it does, and that is a fact. thank you for your research, keep up the good work, I would welcome any response to this comment. God Bless. Sincerely, Thomas Frauenhofer
Hi Monica, i really enjoyed reading your article. it was the most informative I’ve read in a while on the topic of NO. i took some arginine mixed with other things to boost testosterone and increase blood flow to the genitals as well as to the extremities. i noticed that i became extra alert and didn’t need to wear warm clothes (it was a good feeling) but i could not sleep even though i took it 7 hours before bed time. i also had tingling in my left arm that does not go for many hours. also noticed some blurriness in the eyes on a white background. i do have insulin levels that are slightly higher than normal and cholesterol that is bordering the normal range. i’m 38 years old. i would like to continue using arginine and feel that the symptoms of tingling in the extremities will pass and i will regain strong erections which are nowhere like they used to be. what is your advice. BP: 135/90?
The tingling comes from beta-alanine, which is added to most NO boosting supps.
A detailed blood-work could probably explain why you are benefiting from arginine supplementation.
Thanks for the quick response. What do you recommend I get tested? Also I didn’t mention another side effect which is that I urinate much more frequently. Once every 2 hours if not more. It’s like my body is either trying to get rid of the arginine or causing my body to get rid of something else like sugar.
Please again forgive me if i sounded rude it was not my intention, alls i’m saying is keep it simple in regarding explanations and the sort. I wish i was more knowledgeable in the sciences but presently i am not, i will soon attain such verbeage regarding the sciences of it all and then maybe i’ll take it upon myself to educate the lay persons. Simplicity is the key to life, and understanding, as i’ve come to understand! Much thanks.
Well for whatever it’s worth, I think Monica is doing a wonderful job at blending detailed, precise, and informative scientific discourse (for purposes of elucidating the relevant biological processes involved), with direct and unambiguous practical “here’s the take home message” style of conclusions for anyone who has a hard time assimilating a lot of new terminology at once. I also appreciate the proper source citing techniques. Totally professional. Something this industry could use a lot more of in my opinion. It’s far better than the dumbed down (or even worse… pseudo-scientific) stuff that floats around in the lands of internet “bro-science”. So props to you Monica!
I’m a 3rd year undergrad math/physics/engineering student, but my biology and medicinal knowledge lags behind my math and physics. What I’m getting is that elevated ADMA levels are common in individuals suffering from diabetes, high blood pressure, heart disease, and the other listed conditions, and that high ADMA levels interfere with the utilization of dietary L-Arginine for purposes of NO production. Thus this is why people suffering from said conditions may be able to off-set that interference by consuming additional L-arginine. I’m I understanding that correctly?
Also, when you say “half the enzyme reaction max velocity”, did you mean “max reaction rate” ? Being that velocity is typically a vector quantity modeling a change in distance per unit time with respect to a chosen frame of reference? Or is “velocity” (literally speaking) something of concern in some weird sub-branch of chemical kinetics/reaction-rates that shows up in biochem or P-chem or something I haven’t taken yet? I just assumed you meant half the maximum rate of reaction.
what are some natural ways/methods to increase red blood cells and increase blood flow on top of exercising? 🙂
Very nice read. My new word of the day is……….. “panoply”.
I cant remember where I read it, but it stated that the best way to absorb L-Arginine is actually to take L-Citrulline, and it converts via the kidneys? I do see a lot of pre-workouts using L-Citrulline now.
Also I see many others using the L-arginine metabolite(?) agmatine?
You mentioned that nitrate or nitrite supplementation may be a more effective way to boost NO than L arginine. What are effective nitrate or nitrite supplements or what should I look for in a NO booster that is targeted to the nitrate or nitrite pathway. Most seem to rely on L arginine and don’t really list ingredients.
Great article, Monica, as usual! I’m getting close to age 64, have had lifelong sleep apnea and hypertension. Everything is under control, for the most part, but aging is not something I’m doing gracefully, unfortunately. I haven’t priced L-arginine supplements, yet, but are they generally expensive?
Kent, I strongly recommend you a nitrate supplement instead.
See my article on the nitrate-nitrite-NO pathway, and you will find out why:
http://www.brinkzone.com/uncategorized/nitrate-supplementation-ramp-up-the-less-well-known-no-synthesizing-pathway-to-boost-performance-and-health/
Thanks, Monica, for the advice! I’m definitely going to follow-up on it. I read the latest article on nitrates and nitrites and, although the scientific terms weren’t understandable to me, the main points were. Take care.
I’m glad to hear that. If anything is unclear, please let me know.
Do you have any thoughts on whether or not L-Citrulline has any advantage/disadvantage over L-Arginine ?
If you are looking to specifically boost NO production and have no cardiovascular risk factors, neither L-arginine nor L-Citrulline will do you any good, as L-arginine is not rate-limiting for in healthy folks.
However, if you do have cardiovascular risk factors L-Citrulline or L-arginine may help increase NO production and improve endothelial function, and L-Citrulline may be better than L-arginine.
Regarding performance, one study found that intake of 8 g L-Citrulline prior to a chest workout
significantly increased repetitions performed by approximately 53%.[1]
However, another study that L-Citrulline supplementation significantly impaired treadmill time to exhaustion.[2] This is as odds with the finding that L-Citrulline supplementation may increase ATP production by 34% during exercise, as well as the rate of phosphocreatine recovery after exercise by 20%, and reduce perceptions of fatigue.[3]
There is much less research on L- Citrulline than L-arginine, and the long-term safety of L- Citrulline is unknown. More studies are needed to conclusively determine if L- Citrulline may increase performance, as well as its long term safety…
1. Perez-Guisado J, Jakeman PM: Citrulline malate enhances athletic anaerobic performance and relieves muscle soreness. J Strength Cond Res 2010, 24:1215–1222.
2. Hickner RC, Tanner CJ, Evans CA, Clark PD, Haddock A, Fortune C, Geddis H, Waugh W, McCammon M: L-citrulline reduces time to exhaustion and insulin response to a graded exercise test. Med Sci Sports Exerc 2006, 38:660–666.
3. Bendahan D, Mattei JP, Ghattas B, Confort-Gouny S, Le Guern ME, Cozzone PJ: Citrulline/malate promotes aerobic energy production in human exercising muscle. Br J Sports Med 2002, 36:282–289.
I just updated my article on the nitrate-nitrite-NO pathway, which you may find interesting:
http://www.brinkzone.com/uncategorized/nitrate-supplementation-ramp-up-the-less-well-known-no-synthesizing-pathway-to-boost-performance-and-health/
It is far more effective – both in terms of performance and health enhancement – than either L-arginine or L-citrulline.
Monica writes some of the most informative and useful articles in the industry. Thank you!
Aww, it warms my heart to hear that! 🙂
I am 57, have high blood pressure and cholesterol. So from what I have read L Arginine would be beneficial to me. I have been taking a NOS Supplement from 1st Phorm called Alphasurge DRV. It has Arginine Malate and Arginine Sulfate. It is recommended to be taken only before a workout and no more than 4 time a week. Would something that has more Arginine in it be more appropriate? Is there something that you could comment on as far as if it not scam material?
Nitrite consumption has a perfect correlation with colon cancer.